Also known as “breakbone fever.” Dengue fever is a mosquito-borne viral disease caused by the dengue virus. According to the World Health Organization, around 390 million people are affected, with nearly half of the population at risk throughout the world, primarily in tropical and subtropical regions. Dengue symptoms can range from mild to severe, leading to intense muscle and joint pain, and if left untreated, may also result in life-threatening complications.
This article will help you to understand the types of dengue fever, its causes, prevention tips, and available treatments in detail.
Overview
What is Dengue Fever?
Dengue fever is caused Dengue virus(DENV). This virus is transmitted through the bite of Aedes aegypti or Aedes albopictus mosquitoes. These are mostly active during the daytime and mostly bite during early morning or late afternoon.
The Dengue virus is most commonly found in tropical and subtropical regions such as Central and South America, Africa, some parts of Asia, and the Pacific islands.
What are the types of Dengue Fever?
Based on varying severity, dengue fever can be classified into
1. Dengue Fever (Classical Dengue)
It is characterized by high fever, body aches, and rashes, with mild to moderate symptoms lasting 5-7 days (self-limiting).
2. Dengue Hemorrhagic Fever (DHF)
One of the more severe forms of dengue causes bleeding under the skin, nosebleeds, or gum bleeding, which, if not treated, can lead to a low platelet count and organ damage.
3. Dengue Shock Syndrome (DSS)
This is the most dangerous form of dengue; it can cause a sudden drop in blood pressure and, if left untreated, lead to serious complications such as organ failure.
Note: According to the World Health Organization, DHF and DSS are now classified under Severe dengue types
What are the types of the Dengue virus?
The dengue virus has four types—DENV-1, DENV-2, DENV-3, and DENV-4. All have the potential to cause mild to severe illness. How sick a person becomes is determined more by their immune history and genetics than by the specific virus type.
DENV-1: It generally causes high fever with little to no bleeding. Most patients can eat and drink as usual.
DENV-2: Identified by severe pain that interferes with eating and drinking, as well as pale skin, cold extremities, and a weak pulse.
DENV-3: Can cause a sudden drop in blood pressure, severe bleeding, and extreme weakness, making it difficult to consume food or fluids.
DENV-4: The most severe form, characterized by shock symptoms and a significant drop in blood pressure.
What are the Causes of Dengue fever?
Dengue is not transmissible, which means it does not spread from person to person; however, it only occurs when exposed to any of the four dengue serotypes (DENV-1, DENV-2, DENV-3, and DENV-4)
A person can be infected several times, as we are not immune to all 4 serotypes. When an Aedes mosquito bites, it transmits the virus into our body, leading to infection.
Mode of Transmission of dengue
Mosquito bite – The primary cause. After biting someone with dengue, an uninfected mosquito becomes a carrier or vector, which it can then transmit to a healthy person, allowing the virus to enter our body.
Other ways- Either through blood transfusion or organ transplant (rare but possible), or from mother to child—pregnant women with dengue can pass the virus to their baby.
What are Dengue Risk Factors
Some of the risk factors associated with dengue spread include:
- Previous DENV infection: If you have previously been infected with dengue, re-infection with a different type of the virus can complicate the illness. This happens because antibodies from the first infection can help the new virus spread in the body, a process called Antibody-Dependent Enhancement (ADE).
- Rapid urbanization: Social and environmental factors like high population density, human mobility, irregular water supply, and improper water storage practices can raise the risk of dengue.
- Community knowledge and behavior: Lack of awareness and ineffective preventive practices (e.g., improper water storage, keeping stagnant water in plants, lack of mosquito protection) raise dengue risk; active community involvement in vector monitoring and control can lower it.
- Vector adaptation: By adjusting to changing environments and climates, mosquitoes may expand dengue transmission areas.
- Climate change impact: Urbanization, population migration, and changing weather patterns in tropical and subtropical areas can all affect and raise the risk of dengue transmission.
What are the signs and symptoms of Dengue fever?
Dengue fever symptoms may vary depending on the type of fever. It usually appears 4-10 days after a mosquito bite and lasts up to 7-10 days; some of the symptoms include:
- Unexpectedly high fever (up to 40°C or 104°F)
- Severe headaches
- Pain behind the eyes
- Muscle and joint pain
- Feeling tired and weak
- Skin rash (appearing 2–5 days after fever develops)
- Mild bleeding (nose, gums, or easy bruising)
Dengue fever can also come with or without warning signs, along with two to three of the most common symptoms; these include
Dengue Without warning signs
- Nausea and Vomiting
- Low WBC count (leukopenia)
Severe Dengue fever Warning signs
- Persistent Vomiting
- Abdominal pain or tenderness
- Fluid buildup in the tissue layer lining the lung cavity (pleural effusion) or in the abdomen (ascites) in severe cases
- Mucosal Bleeding (bleeding in the soft tissues lining the canals and organs like the reproductive, respiratory, and digestive systems)
- Enlarged Liver <2cm (can be confirmed through Ultrasound whole abdomen)
- Thrombocytopenia, or low platelet count (associated with dengue hemorrhagic fever), can be confirmed through a hematocrit blood test.
- Severe plasma leakage (may be a sign of dengue hemorrhagic fever)
- Sudden Low Blood pressure due to shock (linked with dengue shock syndrome)
- Higher liver AST (aspartate aminotransferase) and ALT (alanine aminotransferase) levels of more than 1000 may be a sign of organ failure and require medical supervision.
- Cold and wet skin (associated with Dengue shock syndrome)
Note: If you notice any of the warning signs, seek immediate medical attention because they indicate a high risk of developing severe dengue.
What are the stages of Dengue fever?
Dengue fever progresses in three stages, each with its own set of symptoms. The table below describes each stage in detail.
| Phase | Duration | Main Symptoms | Other Signs/Warnings |
| Incubation | 4–10 days after a mosquito bite | No symptoms | The virus multiplies in the body silently |
| Febrile (High Fever) | 2–7 days | Sudden high fever, headache, pain behind eyes, body/joint pain, skin rash | Mild bleeding (nose/gums, red spots), flushed face, vomiting, mild stomach pain, tiredness, enlarged liver |
| Critical | 1–2 days after the fever drops | Fluid leakage from blood vessels, changes in blood pressure | Warning signs: severe stomach pain, persistent vomiting, sudden bleeding, swelling in the belly/chest, restlessness or drowsiness, very low platelets, shock. Get immediate medical help if any warning signs appear. |
| Recovery | Several days | Feeling better, more urine, slower heartbeat, normal BP | Platelets and white cells improve; rash may peel or itch |
| Post-Recovery | 1–2 weeks | Energy returns slowly | Mild skin peeling/itching, joint pain, tiredness |
How is Dengue fever diagnosed?
Diagnosis depends upon the symptoms, medical condition, and history of whether they have had an infection in the past or been bitten by any mosquito. The doctor may also do a physical examination by looking for any rash or any other noticeable symptoms.
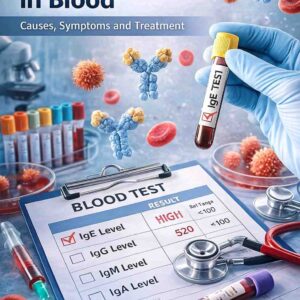
Blood test for dengue fever
Depending on the stage of dengue fever, some of the recommended blood tests are
Early Diagnosis (within 7 days)
NS1 Antigen Test
Detects non-structural protein 1 (NS1), which is released during the early phase of infection and helps confirm early-stage dengue before antibodies develop.
Nucleic Acid Amplification Test (NAAT)
RT-PCR is used to detect Dengue virus RNA (genetic material). And can confirm any active dengue infection with high accuracy.
The Dengue IgM Antibody Test
Identifies and confirms a recent dengue infection by looking for IgM antibodies, which show up 4-5 days after the onset of symptoms.
Note: For a precise diagnosis, the CDC advises performing an IgM anti-DENV antibody test in combination with either an RT-PCR or NS1 antigen test (useful in the first 5-7 days) during the first week of illness.
Later Stages (After 7 Days of Symptoms)
- IgM Antibody Test: The primary diagnostic tool after day 7, as IgM antibodies are detectable for at least three months or longer.
- IgG Antibody Test: Detects IgG antibodies, which typically appear 7-10 days after symptom onset and can persist for years; also checks for previous infection.
Other supporting tests
Complete Blood Count (CBC): Measures platelet, white blood cell, and hematocrit levels to check for low platelet count (thrombocytopenia) and reduced white blood cells (leukopenia) to evaluate disease severity.
Coagulation Profile: Determines the blood’s clotting function, which can be impaired in severe dengue cases.
Note: It’s important to consult with a doctor if you are having symptoms of dengue to ensure proper testing and a treatment plan
Understanding test results: What does a positive dengue test result mean?
The table below can help you understand your test results
| Test / Parameter | Positive / Abnormal Result | Interpretation/Clinical Significance |
| NS1 Antigen or RT-PCR | Positive | Indicates a current dengue infection. |
| IgM Antibody | Positive | Suggests a recent dengue infection. |
| IgG Antibody | Positive | Indicates past dengue infection or exposure (not specific for current illness). |
| CBC – WBC Count | Leukopenia (low white blood cells) on the second day of fever | Common in dengue; aids diagnosis. |
| CBC – Platelet Count | Thrombocytopenia (low platelet count), mild in classic dengue, or a rapid platelet count drop, is a significant warning sign. | It is linked to disease severity. |
| Hematocrit. | A hematocrit increase of more than 20% from baseline indicates significant plasma leakage and warns of severe dengue. | Indicates plasma leakage and risk of severe dengue. |
| Liver Function Tests (LFTs) | AST: ALT ratio > 2 (elevated liver enzymes) | Suggests liver involvement in dengue. |
| Serum Albumin | < 3.5 g/dL (hypoalbuminemia) | Indicates plasma leakage. |
Note: Make sure to get your dengue report checked by a doctor once, so that you are sure what precautions you need to take and how to proceed further if medications are needed.
How to Treat Dengue Fever?
While there is no direct dengue fever treatment, treatment focuses on relieving the pain and inflammation to provide relief and prevent any further complications.
Home Care for Mild Dengue
- Drink plenty of fluids to avoid dehydration.
- Allow yourself as much rest as possible.
- Use paracetamol to relieve fever and pain (avoid aspirin and ibuprofen because they increase the risk of bleeding).
Hospital treatment for severe dengue
- Intravenous (IV) fluid replacement helps restore lost fluids.
- Continuous monitoring for shock, as dengue shock syndrome can cause a sudden drop in BP, which may lead to organ failure.
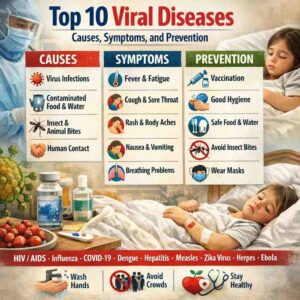
How to Prevent Dengue Fever?
The only way to prevent dengue fever is to protect yourself from mosquito bites and control the mosquito population.
1. Avoid Mosquito Bites
- Use mosquito repellents with DEET, picaridin, or IR3535 as recommended by the World Health Organization.
- Wear full-sleeved shirts and pants.
- Sleep under mosquito nets or spray repellent on them.
2. Control Mosquito Breeding
- Drain stagnant water from containers, flower pots, and tires.
- Keep the water tanks covered.
- Clean and scrub water storage containers once a week.
3. Community Measures
- Areas with poor drainage and sewage systems, fogging, and spraying insecticides can control mosquito rise.
- Spreading awareness and educating communities can help mosquito control.
4. Vaccination
Dengvaxia is an approved dengue vaccine in some countries, but it is only recommended after consulting with a doctor for people who have previously been infected with dengue. Giving it to someone who has never had dengue can increase their chances of developing severe dengue in the future.
What are the complications of dengue fever?
If not diagnosed timely, untreated dengue fever can lead to serious and life-threatening complications such as:
- Severe dehydration brought on by vomiting, a poor fluid intake, and a persistently high fever.
- Thrombocytopenia, or low platelet counts, raises the risk of bleeding.
- Internal bleeding can appear as nosebleeds, bleeding gums, blood in urine or stools, or bruising.
- Organ failure affecting the liver, heart, and other vital organs.
- Death occurs in severe cases, particularly in dengue hemorrhagic fever and dengue shock syndrome.
Key Takeaway:
Dengue fever is a preventable but potentially fatal mosquito-borne illness. Understanding its types, causes, symptoms, and transmission, as well as early detection, prompt treatment, and effective mosquito control, is critical for avoiding complications and protecting both individual and community health.
People may ask.
Can you get dengue fever more than once?
Yes. Because there are four virus strains, a person may contract dengue up to four times in their lifetime.
How long does dengue fever last?
Mild dengue lasts about 5-7 days, but weakness can last for weeks.
Is dengue contagious from person to person?
No. Dengue spreads only through mosquito bites, not through direct human contact.
What foods help in dengue recovery?
Hydrating foods such as coconut water, papaya leaf extract (traditionally used), soups, and fresh fruits aid recovery.
What are the blood tests to diagnose dengue fever?
Tests like the IgM, IgG antibody test, NS1 antigen body test, and RT PCR diagnosis help rule out and confirm the diagnosis of dengue fever.
Do I need any imaging tests for dengue fever?
In case of a severe condition like pleural effusion (fluid buildup in the lung cavity), a chest X-ray may be done to help confirm the lung diagnosis
Can dengue be prevented through vaccination?
The dengue vaccine is available in some areas, but it is not generally recommended for everyone. Consult your physician.
References:-