Overview
What is Fatty Liver Disease?
Fatty Liver Disease (FLD), also known as hepatic steatosis, is a condition characterized by the accumulation of excess fat (more than 5-10%) in the liver. While a small amount of fat in the liver is normal, excessive fat can lead to inflammation and serious liver damage over time. As lifestyle-related diseases rise, fatty liver has become one of the most common liver conditions worldwide, often remaining unnoticed until it causes significant problems.
Fatty vs Normal Liver: Difference
A healthy liver is reddish-brown, smooth, and efficient in filtering out harmful waste, producing bile, and controlling metabolism. When it gets fatty, its texture changes, appearing pale and swollen. Influences liver functioning, making it harder to carry out its normal activities, affecting your overall health.
Understanding Fatty Liver Disease
There are two main types of Fatty Liver Disease
1. Non-Alcoholic Fatty Liver Disease (NAFLD):The most common type happens in those people who drink little or no alcohol and is found to be associated with people with obesity, type 2 diabetes, high cholesterol, and metabolic syndrome.
Subtypes of NAFLD
- Simple fatty liver (steatosis):Inflammation in the liver without fat collection or liver damage.
- Non-alcoholic steatohepatitis (NASH): It causes inflammation and liver cell damage due to fat buildup and may progress to serious liver diseases if untreated.
2. Alcoholic Fatty Liver Disease (AFLD):Affecting people with high alcohol consumption, as the liver breaks down alcohol, producing harmful substances. Excessive levels of it can stress your liver, leading to liver damage and inflammation.
What are the causes of Fatty Liver
- Weight gain
- Having Type 2 diabetes
- Insulin resistance (promotes fat storage in the liver)
- High Blood cholesterol level
- Poor diet with high sugar and saturated fats
- Poor nutrition or rapid weight loss
- Certain medications (like corticosteroids, tamoxifen, and methotrexate)
- Polycystic ovary syndrome (PCOS)
What are the risk Factors for Non alcoholic fatty Liver disease (NAFLD)
- Age—With age, the body’s natural metabolism slows down, increasing the risk of fatty liver condition.
- Sedentary Lifestyle—A person with little or no physical activity has a relatively high risk of getting fatty liver.
- Sleep apnea—A Sleeping disorder causes blockage or narrowing of the airway, leading to low oxygen levels, which may trigger inflammatory and oxidative stress in the liver.
- Genetics—Some people have a higher chance of developing fatty liver due to genes, or the condition, such as Wilson disease, can contribute.
Apart from NAFLD, some risk factors are also associated with AFLD it including:
- Long-term alcohol intake
- Poor diet
- Viral Hepatitis (coexisting)
What are the symptoms of Fatty Liver Disease
These are often comes with silent symptoms because it shows no noticeable symptoms in the early stages; however, as the disease progresses, it may present the following signs:
Early symptoms
- Fatigue and anxiety
- Mild discomfort in the upper abdominal pain
- Slight weight gain
Advanced Symptoms and Complications
- Abdominal Swelling (ascites)
- Yellowing of the skin and eyes (jaundice)
- Enlarged Liver
- Mental Confusion (hepatic encephalopathy)
- Muscle wasting
- Liver failure (in advanced stages like cirrhosis)
What are the stages of Fatty Liver Disease
Fatty Liver progresses in stages.
- Simple Steatosis (Fatty Liver): Fat begins to accumulate in the liver without inflammation or damage.
- Non-Alcoholic Steatohepatitis (NASH): Fat buildup leads to the beginning of inflammation and liver cell damage.
- Fibrosis: Continued Inflammation can cause scarring in the liver.
- Cirrhosis: If scarring continues, it impairs liver function and may lead to liver failure or liver cancer.
How is Fatty liver diagnosed?
Doctors will examine alcohol intake, dietary habits, medications, medical history, and existing conditions like diabetes or hypertension.
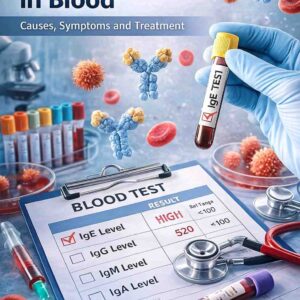
2. Blood Tests
- Liver function tests (ALT, AST) are often elevated in fatty liver.
- Lipid profile—checks for the level of cholesterol and triglycerides.
- Fasting blood sugar and HbA1c—to detect insulin resistance or diabetes.
3. Imaging Tests
- Ultrasound—commonly used to check for grade and fatty infiltration
- CT or MRI – provides more detailed liver images.
- Transient Elastography (FibroScan): evaluates the liver’s stiffness and fat content.
- Liver Biopsy:A small tissue sample is obtained and examined under a microscope to determine inflammation, scarring, and fat content, considered the most accurate test for detecting NASH and liver fibrosis.
What is the treatment of Fatty Liver Disease?
There is no specific medication approved to treat fatty Liver. Adopting good lifestyle habits can help manage or may even reverse the fatty liver condition if followed with the right approach.
Lifestyle Modifications
- Healthy weight:Attempting to lose 7-10% of your body weight can significantly reduce liver fat; it will also help improve your fitness and overall health.
- Diet plan:Follow healthy diet practices such as the Mediterranean diet, which is rich in fruits, vegetables, whole grains, nuts, and healthy fats (olive oil).
-
Exercise regularly:Aim for 150 minutes of moderate-intensity activity per week, such as walking or cycling. You can also go for Resistance training to improve insulin sensitivity.
- Liver Transplant :In case of advanced liver disease like cirrhosis, which causes liver failure, transplanting may be the only option.
- Medications:Some medications may benefit indirectly by reducing inflammation or other risk factors that can lead to fat accumulation.
- Vitamin E: Can improve liver inflammation in non-diabetic patients.
- Pioglitazone: A diabetes drug that may benefit NASH.
- Statins: They help lower cholesterol levels (for NAFLD patients).
- Metformin—Used in insulin resistance and type 2 diabetes.
- Obeticholic acid (OCA)—under clinical trials for NASH treatment.
Note: The above medications mentioned are intended for educational purposes only and doctor (liver specialist) consultation is required before using.
How to prevent fatty Liver disease?
Here are some of the tips to keep your liver healthy; these include:
- Maintain a healthy body weight.
- Limit or avoid alcohol intake if you have a high chance of getting fatty liver.
- Manage the underlying conditions such as high Blood pressure, diabetes, and cholesterol.
- Don’t take any medications or supplements without consulting your doctor; it may stress your liver.
- Go for regular health checkups.
When to see a doctor
Go to a doctor. If you experience the following symptoms,
- Chronic fatigue or weakness
- Abdominal discomfort.
- Yellowing of the skin and eyes
- Unexplained weight loss
- If the blood test shows elevated levels of liver enzymes like ALT and AST
What questions to ask a Doctor
Seek medical attention if you:
- Feel weak or tired all the time.
- Notice yellowing of the skin or eyes.
- Feel swollen in the legs or abdomen
- Experience unexplained nausea or weight loss
- Have metabolic disorders or a family history of liver disease
Final Thoughts
Fatty liver disease is a silent epidemic, but it is largely preventable and treatable. You can protect your liver and overall health by adopting a healthy lifestyle, seeking medical attention, and continuing to monitor your condition.Whether you are at risk or have already been diagnosed, taking action now can help you avoid complications later. Talk with your doctor about your liver health, get tested if you’re in a high-risk group, and work toward a healthier, liver-friendly lifestyle.
FAQs
What are the early warning signs of fatty liver disease?
Fatty liver disease frequently has no symptoms in its early stages. However, some people may experience fatigue, mild abdominal discomfort (particularly on the upper right side), unexplained weight loss, or a general sense of unwellness. Regular screening is important if you have risk factors like obesity or diabetes.
Can fatty liver disease be reversed?
Yes, in many cases, fatty liver disease, particularly non-alcoholic fatty liver (NAFLD), can be reversed through lifestyle changes. Weight loss, a healthy diet, regular exercise, and controlling blood sugar and cholesterol levels can all help to reduce fat in the liver and improve function.
How is fatty liver disease diagnosed?
Fatty liver is typically diagnosed through a combination of blood tests, imaging (such as ultrasound, CT, or FibroScan), and, in some cases, a liver biopsy. Liver function tests may reveal elevated enzyme levels, but imaging confirms fat accumulation.
What foods should be avoided with fatty liver disease?
People with fatty liver should avoid:
- Drink with high calorie and refined sugars
- White bread, rice, and pasta
- Fried and fatty foods
- Processed food and red meats
- Alcohol (completely, especially in AFLD)
Instead, focus on whole grains, lean protein, vegetables, fruits, and healthy fats like those in nuts and olive oil.
Is medication available for fatty liver treatment?
There are currently no FDA-approved treatments for fatty liver disease. However, doctors may prescribe medications to treat related conditions such as diabetes, high cholesterol, or obesity. Certain supplements, such as vitamin E or experimental drugs, may be used under supervision.